Dr. Annie De Groot ’78: Designing a Vaccine
Alum News

Published April 8, 2020 (UPDATED: June 15, 2020)
When scientists in China released the gene sequence for the novel coronavirus, Dr. Annie De Groot ’78 and her team at EpiVax, the Providence, Rhode Island–based biotech firm she co-founded in 1998, got to work doing what they do best—developing a vaccine to combat the virus.
It’s a moment, De Groot says, for which she and her company have been preparing for more than two decades. As an infectious disease specialist, De Groot is widely known for her use of mathematical modeling and computer science to chart the body’s response to pathogens—including bird flu, HIV and tuberculosis—and, thus, produce vaccines to mitigate serious diseases, especially among vulnerable populations.
The work De Groot and her EpiVax colleagues—including Frances Terry ’06 and Dr. Christine Swymer Boyle ’90—are doing now in the fight against COVID-19 is focused on designing a vaccine that uses fragments of proteins, or peptides, that look like the virus. The body’s immune cells then learn to seek out and destroy anything carrying those peptides. Though peptide-based vaccines don’t prevent infection, they greatly reduce the severity of illness by helping the body fight infection, which at this point, De Groot says, is an important tool in our arsenal that could “buy us some time” and help frontline health care workers.

Annie De Groot ’78, far right, and her team of vaccinologists at EpiVax, including Christine Swymer Boyle ’90 and Frances Terry ’06, middle row, third and fourth from right.
In April, De Groot took some time to discuss the impact of COVID-19, how it compares to other headline-making diseases and what we need to look out for once a vaccine is ready for use.
Cases of COVID-19 now number in the millions in the U.S. Given our experience with other pandemics and epidemics, was this avoidable? Should we have been better prepared?
This crisis was undoubtedly avoidable. We should have started mobilizing with testing, equipment and strategies when the news of the virus first came out of China. In addition, our “just in time” economy has made it challenging to stockpile things like personal protection equipment and ventilators and drugs. Our economy is built to provide those things on an “as needed” basis. That’s a great system for reducing costs, but not so great when you have a spike in demand such as the one caused by this pandemic.
We’ve had epidemics in recent years—H1N1, Zika, SARS—that have caught the public’s attention, but not nearly as much as COVID-19. What’s different this time?
COVID-19 is highly contagious. It has an infection rate of 2.2, meaning that each infected person will spread it to 2.2 other people. This is significantly higher than SARS or Zika. In addition, many infected people are asymptomatic. They are often out and about in the community, spreading the virus without even knowing they are sick. COVID-19 is also not yet treatable, and because it is a novel virus, we do not have any natural immunity to it.
In your experience as an infectious disease specialist, what concerns you the most about COVID-19?
It poses a real risk to our health care system. Health care providers lack basic protective equipment, and hospitals in epicenters are ill-equipped to deal with the number of people who need high levels of care. Once a person is admitted to the hospital, his or her stay is likely to be 10 to 14 days. That’s a long time for that bed to be unavailable. Providers are being forced by circumstances to make unimaginable choices about who gets care and who doesn’t. People on the margins— the uninsured, the homeless, the undocumented—are particularly vulnerable.
Where are you in the process of developing a vaccine?
Right now, we are working on nine different vaccines with an international assembly of collaborators. The projects vary based on the design of the vaccine, the delivery method and the way they influence the immune system.
Are you working on any vaccine candidates that are particularly exciting?
Some of the most promising projects are T cell–directed vaccines. These vaccines stimulate the immune system to produce CD4 T helper cells and CD8 T cells, both of which are involved in protective cellular immunity. This reduces viral load, and thus reduces symptoms. One of those projects is our own vaccine, which is also a T cell–directed vaccine.
“Our advanced tools are accelerating the development of a safe and effective vaccine that could be ready sometime in the fall.”
Why do you find this approach so promising?
It is particularly promising because it is already known to be a safe approach in humans, so the time it takes for approval could be markedly shorter than the years required by more traditional approaches. We’ve started to submit the paperwork and to coordinate the phase-one safety trial for this vaccine. We believe that we could get started within three months of receiving funding.
Are there obstacles that make it harder for EpiVax to do its work?
Funding is the biggest obstacle. We need $1.75 million to begin our work and $3.25 million to start a phase-one trial. The entire process of getting the vaccine to the clinic will take $10 million due to the cost of running large phase-three trials, mainly due to the work associated with measuring the impact of the vaccine on immune response to the virus.
Realistically, how far away are we from a successful vaccine?
Our advanced immunoinformatics tools are accelerating the development of a safe and effective vaccine that could be ready sometime in the fall. Funding is the impediment, but I am a Smithie and I don’t let the usual obstacles daunt my optimism. If there are any Smithies out there who could be helpful, please reach out through my email: Dr.Annie.DeGroot@gmail.com.
Your approach to vaccine development, and health care in general, has a strong social justice foundation. From that perspective, what are your concerns about the way this pandemic is being managed right now?
Accessing the health care system is difficult for the poor, the homeless and the underinsured in the best of times. In an environment where health care resources are scarce, vulnerable populations will be the first to suffer and the last to get relief. We need to ensure equitable access to treatments.
Your motto at EpiVax is “science without fear.” What can you say that might allay people’s fears right now?
We are scientists. We are vaccinologists. We got this. Scientists all over the world are collaborating to fight this virus. That’s a beautiful thing.
This story appears in the Summer 2020 issue of the Smith Alumnae Quarterly.
A Semester Like No Other: How the class of 2020 left campus with a proper send-off.
Smith’s All-Hands Crisis Response: Entire campus community takes up an array of challenges presented by a dangerous pandemic.
Connection Out of Isolation: 12 voices collaborate on a poem for our time.
Mission to Make Masks: Students, staff rev up sewing machines to fill a community need.
One Student: Studio art major Sophie Willard Van Sistine ’22 finds her niche writing comics.
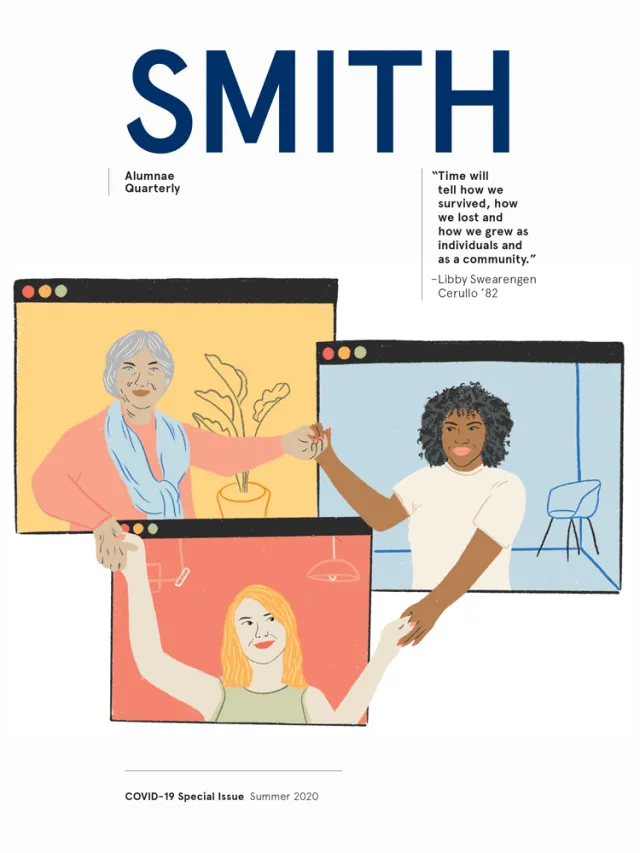
Virtual Togetherness: Quarantines fall away as Smith friends Zoom into one another’s living rooms.
Echoes of a Pandemic: From canceled classes to campus quarantines, effects of the 1918 Spanish flu ring familiar.
Finding the Funny: An improv comedian’s tips for staying sane in the pandemic.
How Can I Help? From online classes to concerts and community fundraisers, alumnae find creative ways to ease the burden of those in need.
Feeling Community Through My Window: Teresa Kábana ’92 sends a dispatch from Madrid.
The Morning Call That Never Came: Death of a parent in the age of COVID-19 carries an extra layer of grief.
Racialization of Infectious Disease: As viruses spread, so does discrimination against marginalized groups.
Dawn of a New Day: Faith leaders impart messages of hope, acceptance and belief in our collective power to work for a better world.